“The advance of genetic engineering makes it quite conceivable that we will begin to design our own evolutionary progress.”
“The advance of genetic engineering makes it quite conceivable that we will begin to design our own evolutionary progress.”
~Isaac Asimov, famous thinker and sci-fi writer
Cornell University researchers in New York revealed that they had produced what is believed to be the world’s first genetically altered human embryo—an ironic twist considering all the criticism the US has heaped on South Korea over the past several years for going “too far” with its genetic research programs. The Cornell team, led by Nikica Zaninovic, used a virus to add a green fluorescent protein gene, to a human embryo left over from an in vitro fertilization procedure. The research was presented at a meeting of the American Society of Reproductive Medicine last year, but details have emerged only after new controversy has emerged over the ethics and science of genetically modifying humans.
Zaninovic has pointed out that in order to be sure that the new gene had been inserted and the embryo had been genetically modified, scientists would ideally want to keep growing the embryo and carry out further tests. However, the Cornell team did not get permission to keep the embryo alive. The GM embryos created could theoretically have become the world’s first genetically altered man or woman, but it was destroyed after five days.
British regulators form the Human Fertilization and Embryology Authority (HFEA), have warned that such controversial experiments cause “large ethical and public interest issues”.
Much of the debate stems from the fact that the effects of genetically altering an embryo would be generational and permanent. In other words, if we create a mutant baby and it grows up to have children of it’s own—they’ll all be mutant gene carriers too. Genes injected into embryos and reproductive cells, such as sperm, affect every cells in the body and would be passed on to future generations. Critics say current humans don’t have the right to tamper with the gene pool of future generations.
On the other hand, proponents of such technology say that this science could potentially erase diseases such as cystic fibrosis, hemophilia and even cancer. In theory, any “good” gene could be added to embryos to offset any “bad” genes they are currently carrying. That could potentially mean the difference between life and death for many children.
John Harris, the Sir David Alliance Professor of Bioethics at Manchester University, takes it a step further. He believes that as parents, citizens, and scientists, we are morally obliged to do whatever we can genetically to make life better and longer for our children and ourselves. Society currently devotes so much energy and resources towards saving lives, which, in reality, is simply postponing death, he notes. If it is right to save life, Harris reasons, then it should also be right to postpone death by stemming the flow of diseases that carry us to the grave.
For Harris, having the ability to improve our species lot in life but refusing to do so, makes little sense. He has a difficult time understanding why some people are so insistent that we shouldn’t try to improve upon human evolution.
“Can you imagine our ape ancestors getting together and saying, ‘this is pretty good, guys. Let’s stop it right here!’. That’s the equivalent of what people say today.”
Ethicists, however, warn that genetically modifying embryos will lead to designer babies preloaded with socially desirable traits involving height, intelligence and coloring.
Dr David King, director of Human Genetics Alert, warns, “This is the first step on the road that will lead to the nightmare of designer babies and a new eugenics.”
Harris, however, doesn’t support that argument. He says it’s not about “beauty” it’s about health, and what parent wouldn’t want a healthy child, he asks.
“Certainly, sometimes we want competitive advantage [for our children], but for the enhancements I talk about, the competitive advantage is not the prime motive. I didn’t give my son a good diet in the hope that others eat a bad diet and die prematurely. I’m happy if everyone has a good diet. The moral imperative should be that enhancements are generally available because they are good for everyone.”
The only other route to equality, he says, is to level down so that everyone is as uneducated, unhealthy and unenhanced as the lowest in society – which would be much more unethical in his opinion. Even though we can’t offer a liver transplant to all who need them, he says, we still carry them out for the lucky few. “Much better to try to raise the baseline, even if some are left behind.”
The Human Fertilization and Embryology Bill in currently under consideration in Britain will likely make it legal to create GM embryos in that country, but only for research—implantation in the womb will still be banned—at least for now. However, ethicists believe that the legislation could easily be relaxed even further in the future.
People who believe that genetically modified humans is something way into the future might want to consider that many experts are worried that some forms of it are already happening in the sports world.
Faster, bigger, better, stronger—in theory, the single most effective way to radically alter your physical capacities is to manipulate your genes. Athletes are beginning to take notice. Now that we’ve mapped out the human genome and identified exactly which genes make you buff, tough and rough—experts are concerned about the future of genetic doping.
Gene doping could spawn athletes capable of out-running, out-jumping and out-cycling even the world’s greatest champions. However, researchers at the University of Florida are attempting to prevent that from happening by detecting the first cases of gene doping in professional athletes before the practice becomes mainstream.
Montreal-based World Anti-Doping Agency (WADA), responsible for monitoring the conduct of athletes, is working with investigators around the globe to develop testing to identify competitors who have injected themselves with genetic material that is capable of enhancing muscle mass or heightening endurance.
“If an athlete injects himself in the muscle with DNA, would we be able to detect that?” asked one of France’s leading gene therapy researchers, Philippe Moullier, M.D., Ph.D., director of the Gene Therapy Laboratory at the Universite de Nantes in France.
Right now, he says the answer is clearly “no”. But that may soon change. The UF scientists are among several groups collaborating with national and global anti-doping organizations to develop a test that can detect evidence of “doped” DNA.
“WADA has had a research program in place for some years now, to try to develop tests for gene-based doping,” said Theodore Friedmann, M.D., head of the agency’s panel on genetic doping and director of the gene therapy program at the University of California, San Diego.
Nearly every day now we are inundated with new genetic discoveries. Scientists can now pinpoint many specific genes including being lean, living a long life, improved self-healing, thrill seeking behavior, and having an improved memory among many other incredible traits. Many believe that these genes can be manipulated in ordinary humans, in effect creating Super-Mutants.
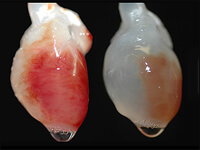
Theoretically, options are nearly limitless. Even a gene that exists in another species could be brought over to a human cell. Imagine some of the incredible traits of the animal kingdom that some humans don’t possess such as night vision, amazing agility, or the ability to breath underwater. The precedence for these types of radical changes is already in place. Experimental mice, for example, were successfully given the human ability to see in color. If animals can be engineered to have human traits, then humans can certainly be mutated to have desirable animal traits.
It is even thought possible to so drastically alter human genomes that a type of superhuman species could emerge. The fear with germline engineering is that since it is inheritable, offspring and all succeeding generations would carry the modified traits. This is one reason why this type of engineering is currently banned- it could lead to irreversible alteration of the entire human species.
Ethics, not scientific limitations, is the real brick wall. Most scientists believe manipulating genes in order to make an individual healthy is a noble and worthwhile pursuit. Some are against even that notion, arguing that historically amazing individuals have sometimes been plagued by genetic mental and physical disorders, which inadvertently shaped the greatness of their lives. Should we rob the human race of character shaping frailty? Very few scientists would dare to publicly endorse the idea of using genetic engineering to make a normal, healthy individuals somehow superior to the rest of the human race.
“The push to redesign human beings, animals and plants to meet the commercial goals of a limited number of individuals is fundamentally at odds with the principle of respect for nature,”
said Brent Blackwelder, President of Friends of the Earth in his testimony before the Senate Appropriations Committee.
However, would it be so bad if the human race were slightly improved? What if a relatively simple procedure could make an individual and his or her offspring resistant to cancer? After all, Nature isn’t always right. Nature has naturally selected many people to carry the burden of uncomfortable and often lethal genetic disorders. If nature knows best, then shouldn’t we quit trying to “improve” upon nature by “curing” people of genetic conditions we consider inferior? Many say we shouldn’t change human genetics, UNLESS it’s the RIGHT thing to do. Who gets to decide where the line is between righteous endeavor and the corruption of nature? These are the questions facing our generation.
Posted by Rebecca Sato